Birth control is broad term referring to both medications and devices that can prevent pregnancy and provide therapeutic relief for a number of common health issues, including acne, premenstrual syndrome, and heavy or painful periods. For many individuals, the use of “birth control” has nothing to do with reproduction. Similarly, although “birth control” is culturally synonymous with use by cisgender, heterosexual women, it is also regularly used by folks of many other gender identities and sexual orientations. LGBTQ+ individuals can have a variety of possible partnerships and family planning needs and therefore, may or may not desire the use of a pregnancy prevention method. In order to help your provider identify your healthcare and birth control goals, it is beneficial to share as much as possible in your sexual history.
As Planned Parenthood nurse Kaity Molé explains, when visiting your GYN care provider, “It is helpful to be as open and detailed as possible when discussing your sexual health and activities,” including “what body parts or body fluids your partner(s) have and how/if you’re exposed to them, in order to better understand your risk for pregnancy and/or STIs and help you choose a method that works well for you.” This is an important distinction because a patient may report identifying as a lesbian and sleeping with only women, but her partner may be a transwoman who produces sperm, making the possibility of pregnancy would still be present.
However, Molé added, “Since it can feel invasive when a clinician is asking personal questions about you, your partner(s), or the sex you have/don’t have, it’s your choice what you share and it’s okay to choose not to answer certain questions until you’re comfortable.” It’s also important to note that the historical context surrounding the use of birth control is both complex and associated with the coercion of vulnerable populations. Therefore, remember the choices you make surrounding your health and your bodily autonomy are yours alone and should always be respected by your healthcare provider.
So what are the options for folks who have a uterus and/or ovaries?
Combined Hormonal Methods: The Pill, Patch, and Ring
The most well-known method is the birth control pill, also called the oral contraceptive pill (OCP). These medications contain a combination of two hormones: estrogen and progesterone. The primary mechanism of the pill is to prevent ovulation–or the release of the egg from the ovary–an event necessary for conception to occur. OCPs also thicken cervical mucus in the cervix, which blocks the sperms’ pathway to the egg.
“Some positive things that people may like about the pill are that it often lightens bleeding, decreases cramping and premenstrual symptoms, can provide some protection against ovarian cancer, and helps give you control over when your period arrives each month,” Molé says. “You can also talk to your clinician about taking these pills in way that makes you not bleed at all, because bleeding each month is not something that is medically necessary.”
One downside to the pill is that it needs to be taken daily, which can be hard for some people. Some folks experience side effects on the pill such as mood changes, bloating, spotting, and headaches. Often, these effects reduce in severity or resolve completely within the first few months.
The pill is not recommended for anyone who experiences migraine headaches with visual changes, is over 35 and smokes cigarettes, has uncontrolled high blood pressure, liver or breast disease, those with a history of blood clots, or other health conditions. There is also a pill that contains only progesterone and not estrogen, which can be more appropriate for those who have the above medical contraindications to estrogen. However, it must be taken within a very narrow window each day and late or missed doses will require a backup method. Either pill can be stopped at any point if a person no longer needs it or is experiencing side effects that do not resolve.
Like the pill, the ring and the contraceptive patch contain both estrogen and progesterone. These options can be helpful for folks who have trouble remembering to take a daily medication. The ring is a flexible piece of plastic that sits in the vagina for three to four weeks at a time. The patch is applied directly to the skin weekly. Both release hormones locally, which are then absorbed and circulated throughout the body.
It is important to note that while the absolute risk is low, any estrogen-containing medication does carry an increased risk of blood clots, so it’s important to discuss your personal risks with your provider.
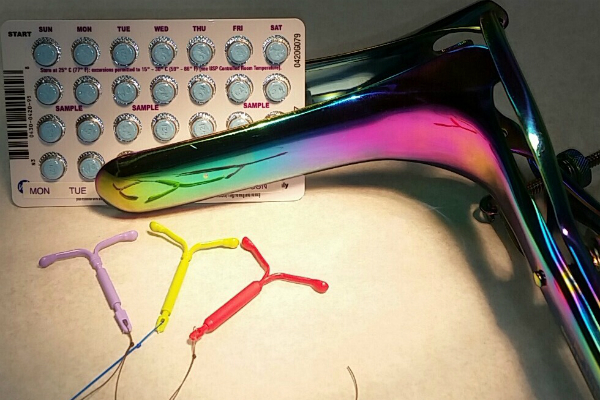
IUDs
Intrauterine devices (IUDs), often referred to as long-acting reversible contraception (LARC), are an increasingly popular option for contraception and for managing common issues such as heavy or painful periods. There are two categories of IUDs: hormonal IUDs, which slowly release progesterone (Mirena, Skyla, Liletta and Kyleena) and non-hormonal IUDs (Paragard). Both types are over 99 percent effective at preventing pregnancy and allow immediate return to fertility after removal, thus allowing the person to get pregnant within the first cycle after the device is taken out. Paragard offers a highly effective, non-hormonal contraceptive option and the hormonal IUDs offer multiple benefits in addition to pregnancy prevention, including decreased menstrual cramping, lighter periods, and in some cases, complete cessation of periods.
The insertion experience for both types of IUDs can range from mildly uncomfortable to painful, but the entire process only takes a few minutes to complete. Afterward, cramping may be experienced but it is generally mild and resolves within a few hours to a few days. Individuals who have never given birth are more likely to experience stronger cramping and discomfort, but ibuprofen usually provides adequate pain-relief.
Hormonal IUDs, which release progesterone locally within the uterus, thickens cervical mucus and may also reduce the likelihood of ovulation. After insertion, hormonal IUDs last between three and five years before needing to be replaced. A very common side effect of hormonal IUDs is irregular spotting and bleeding for the first three to six months after insertion, which can be bothersome to some folks. After this time though, bleeding patterns typically become regular and up to 20 percent will stop getting a period by the end of the first year of use.
Paragard, the non-hormonal IUD, prevents pregnancy by acting as a spermicide and may also prevent implantation. This type of IUD is approved for 10 years of use and can be a good choice for those who want or need to avoid hormones. Individuals typically follow the same menstrual pattern they had prior to insertion, but periods may be heavier with increased cramping, so this option is generally not recommended if a person already has heavy or painful periods.
IUDs are contraindicated in a number of circumstances including current pelvic infection, fibroids that distort the uterine cavity, and any condition in which progesterone is contraindicated, such as liver disease or breast cancer. Because it contains copper, Paragard is also contraindicated in individuals with a copper allergy.
The Implant
Another LARC option, the implant–called Nexplanon in the U.S.–is a small plastic implant about the size of a matchstick that is placed in the upper inner arm by a clinician. The implant slowly releases a type of progesterone throughout the body, which helps prevent ovulation. It also thickens cervical mucus, which helps prevents sperm from reaching eggs. Side effects are the same as the hormonal IUD and usually involve up to six months of irregular bleeding or spotting.
The benefits of Nexplanon include being over 99 percent effective for pregnancy prevention and allowing a less invasive insertion process than an IUD. Insertion involves the use of a local anesthetic to numb the area, a small incision, and placing the device beneath the skin. The process only takes a few minutes and patients typically describe it as mildly uncomfortable. Contraindications are similar to those of the hormonal IUD.
The Injection
The contraceptive injection, known as Depo-Provera, contains a type of progesterone and is administered every three months. It has a relatively high level of efficacy for pregnancy prevention and only requires patients to remember their birth control four times a year. Side effects are similar to other progesterone-only containing methods, though once injected, the effects can continue for the next three months. Depo-Provera is also associated with weight gain, depression, and an increased risk of bone density loss, which can put a person at risk for fractures or osteoporosis. Because of this, patients using Depo-Provera are encouraged to take a calcium supplement and not use this method long-term.
Progesterone-Only Options
Progesterone-only methods such as progesterone-only pills, hormonal IUDs, Nexplanon, and Depo-Provera can be particularly appropriate for those taking testosterone, as progesterone does not interfere with the gender-affirming effects of the medication. Similarly, for those not on testosterone but experiencing dysphoria during periods, choosing a method most effective at suppressing a period may be helpful. Chat with your clinician to find a choice that fits your needs.
Fertility Awareness Method
Fertility Awareness Method (FAM) refers to pregnancy prevention through menstrual cycle tracking and without the use of contraceptive medications or devices. While many people are familiar with the notoriously ineffective “calendar method,” which relies on false assumptions regarding ovulation timing the, highly-effective FAM is lesser known. This involves tracking one’s menstrual cycle and identifying the signs of ovulation in order to avoid unprotected sex during fertile periods. Signs of fertility include subtle changes in one’s basal body temperature, movement of one’s cervix, and a noticeable increase in vaginal secretions, which happens in the days leading up to ovulation.
Benefits of this approach include avoidance of potential hormonal side effects and increased bodily awareness. Many people also report a sense of self-empowerment from increased body literacy. Disadvantages include a lower efficacy for typical use and a lower level of reliability for individuals with irregular menstrual cycles or certain conditions that affect cervical fluid like polycystic ovarian syndrome (PCOS). When starting the FAM, it is important to thoroughly educate oneself on the complexities of cycle tracking and spend several months observing and documenting one’s menstrual patterns before solely relying on this method.
If you have questions about your individual health needs and goals, schedule an appointment with your healthcare provider to discuss which options might be best for you.
Signey Olson is a DC-based nurse practitioner and nurse-midwife whose work focuses on providing inclusive care to her queer community. She works primarily in GYN, fertility, and trans-affirming care at Columbia Fertility Associates.